Reproductive Health Knowledge and Services Utilization among Rural Adolescents in Rwamagana District, Rwanda
Abstract
This study aims to assess reproductive health knowledge and services utilization among adolescents from Rwamagana District. A community based cross-sectional study was carried out in Rwamagana district. A sample of 392 adolescent aged 15-19 participated in the study. Simple random sampling was used to select respondents. Data was collected by using a questionnaire adopted from previous studies. Data was checked for completeness, cleaned, coded and entered into excel sheet, and then exported to SPSS version 22.0 for further analysis. Frequencies and percentage was used to summarize descriptive statistics. To determine the association between different factors associated with reproductive health knowledge and services utilization, a logistic regression model was employed. Ethical clearance was obtained from the Ethical committee of Mount Kenya University. It was observed that the majority of adolescents in Rwamagana District knew the sign of maturity. Overall the majority of adolescents 91.8% in Rwamagana District had good knowledge about reproductive health services. The majority of adolescents in Rwamagana District (66.8%) had ever utilized reproductive health services at health facility. It was observed that adolescents who live with their parents were more likely to use reproductive health services compared to those who do not live with parents (aOR=2.161, 95%CI: 1.162-4.021, p=0.015). Moderate reproductive health services utilization was observed among adolescents. There is a need to increase adolescent’s awareness on the available services at health facilities.
Author Contributions
Academic Editor: Lucio Mango, Italy
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2022 Patricie Mukandagano
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
According to World Health Organization (WHO), adolescents are people between 10 and 19 years of age. Today there are 1.2 billion adolescents worldwide with nearly 90% of them living in developing countries. Adolescence is characterized by significant physiological, psychological and social changes that put adolescents for high risk sexual and reproductive health (SRH) problems. This has partially been because adolescents were considered to be relatively healthy, without a heavy “burden of disease” 1, 2.
Adolescents are not quite capable of understanding complex concepts, or the relationship between behaviors and consequences, or the extent of control they have or can have over health decisions making including that related to sexual and reproductive behavior. This makes them vulnerable to sexual exploitation and high-risk sexual behaviors and reproductive health problems 2, 3.
Previous studies demonstrated that the age at marriage for adolescents living in rural areas is quite low compared to their counterpart in urban area. For girls these situations predispose them to teenage pregnancy that may have more immediate effect on their life that any other problem. The changing moral & social values and shift in the standard of societal behavior from conservatism to liberal interaction between both sexes is attributed largely to exposure to the media especially television and movies. Adolescents find themselves sandwiched between a glamorous western influence and a stern conservatism at home, which strictly forbids discussion on sex. This dichotomy aggravates the confusion among adolescents have led to increase in premarital sexual activity, pregnancy among unmarried girls apart from the increasing incidence of abortion & STDs.
Early and unprotected sexual activity and misconceptions about HIV/AIDs are prevalent among rural adolescents4. It was previously reported that adolescent knowledge about sexual reproductive health affects the reproductive health services utilization5. The World Health Organization (WHO) estimates that in Africa, 60% of all new HIV-infection occur in adolescents who are 15-19 years old. In developing countries, there are about 12.8 million births by adolescents aged between 15-19 years, and a large proportion of these pregnancies are unplanned 6.
Adolescent’s sexual and reproductive health knowledge include knowledge about the female menstrual cycle and conception, ways to avoid pregnancy, methods of contraception, correct use of condoms and oral contraceptives, sexually transmitted infections and HIV, means of STIs transmission, ways to avoid STIs and symptoms of STIs. Those are the indicator that used to measure knowledge about SRH 1.
A study conducted in Nigeria found that about half (51.0%) of the respondents had ever used SRH services. The same study showed less than 50% of adolescent were knowledgeable about STIs while 52.9% were knowledgeable about how to avoid unwanted pregnancy. Factors related to adolescent sexual and reproductive health knowledge were being male, having regular cell phone and access to internet 7.
One of the major causes of the high prevalence of STIs among the adolescent is poor utilization of sexual reproductive health services as well as poor knowledge. In developing countries, 20,000 girls of between 15 and 19 give birth every day, One-third these girls are married before 18 years old. Most of them are poor, less educated and living in rural areas 2.
Data from Rwanda’s Ministry of Health indicate that adolescents and young adults comprise the majority of Rwanda’s population. For instance, young adolescents (10-14 years) make up about 17.1%, old adolescents (15-19 years) about 12.4% and young adults comprise 10.7% of the total population while another third of the population (32.1%) is under 10 years. The report showed that adolescents remain neglected group, in the country’s health care model this group is neglected because they are considered comparatively healthy with a low disease burden. Yet the choices adolescent make today affect their health and the health of their families in future, especially the choices related to family planning and STDs. It was reported that Rwandan adolescent lack the ability to negotiate safer sex or to seek the health of family planning services 8.
Due to the lack of knowledge and poor utilization of reproductive health services the number of unwanted pregnancies and STDs has been increasing in Rwanda. The number of teenage pregnancies in various parts of the country shows how government and parents need to put in more efforts to contain the issue which leads many young girls to drop out of school. For example, in 2016 some 17,000 young girls most of them under 18 years got pregnancy 9.
Teenage pregnancy has been described as a major challenge to Rwanda whose numbers are increasing, especially in the rural areas. Poor rural girls with limited or no access to sexual reproductive health services are at higher risk of becoming pregnant or falling victims to sexually transmitted diseases. On other hand, a report from UNICEF showed that young people in Rwanda remain at risk of contracting HIV virus , this is because a large number of young people in Rwanda, are unaware of the risks associated with HIV and particularly how to prevent against HIV. The same report showed that only 49% of males and 43% of female understand how to use condoms 10.
Knowledge and the utilization of reproductive health services are the important components in preventing adolescents from different sexual and reproductive health problems. Limited studies on adolescent knowledge and reproductive services utilization have been conducted in Rwanda. These studies were carried out mainly in urban areas among the general population. Therefore assessing factors affecting reproductive health services utilization within adolescent are very important to improve adolescent reproductive health services utilization and thereby reduce the burden of adolescent disease and disabilities associated with reproductive health.
Methods
Research Design
A community cross-sectional study with quantitative approach was carried out in Rwamagana district. A cross-sectional research design was chosen because this help researcher to collect quick information and make analysis that respondent to study objectives.
Study Area
The present study was conducted in Ramagana district. The district have 14 sectors including Fumbwe, Gahengeli, Gishali, Karehe, Kigabiro, Muhazi, Munyaga, Munyiginya, Musha, Muyumbu, Mwulire, Nyakaliro, Nzige, Rubona. Ten of these sectors do not have urban area. This study was carried out among adolescent from pure rural sectors.
The least populated district in eastern province is Rwamagana with about 313 thousand inhabitants. However, the district is ranked number one with high population density (460 inhabitants/km2). Rwamagana district population is predominantly rural. 91.4% of the resident population (313,461inhabitants) lives in rural areas whereas only 8.6% lives in urban areas. Kigabiro is the most urbanized sector of Rwamagana district with 55% of its population residing in urban areas. It is followed by Karenge (22.2%) and Gishari (7.7%).
Target Population
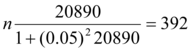
This study was conducted in rural sectors of Rwamagana District. According to fourth population and housing census, the population of Rwamagana is mostly young where 65 % of the resident population of Rwamagana is under 25 years old. Adolescent aged 15-19 years are 31852; of them 20890 are from rural sectors, therefore, this was considered as target population in the present study.
Sample Design
Sample Size Estimation
Sampling Technique
Due to the nature of the study, the study was conducted in rural sectors as the aim of the study is to assess the reproductive health knowledge and services utilization among adolescents from rural areas of Rwamagana District. Table below shows the number of adolescents that selected in each sector. Proportion to sample was used to estimate the respondents from each sector Table 1.
Table 1. Sample size from each selected sector| Sectors | Total Number of adolescent aged 15-19 | Sample size |
|---|---|---|
| Fumbwe | 2325 | 44 |
| Gahengeri | 2365 | 44 |
| Munyaga | 1623 | 31 |
| Munyiginya | 1670 | 31 |
| Musha | 1997 | 37 |
| Muyumbu | 2482 | 47 |
| Mwulire | 2205 | 41 |
| Nyakaliro | 2073 | 39 |
| Nzige | 1740 | 33 |
| Rubona | 2410 | 45 |
| Total | 20890 | 392 |
A total of 392 eligible adolescents were recruited using simple random sampling. All adolescent from the selected sectors had equal chance to be selected. A household with an adolescent aged 15-19 will be used as a sample frame, in case that a household had two or more adolescents, one was selected randomly. Eligibility criteria include: (1) residence of selected sector for at least one year, (2) being in selected sector during data collection period (3) received a consent form from parents or caretaker (4) able to communicate with researcher. All respondents who do not meet the above mentioned criteria were excluded in the study.
Data Collection Instruments
Data was corrected by using a questionnaire. Pre-tested structured questionnaires were prepared by reviewing previous studies on the problem of interest 3, 7. The questionnaire explores the demographic, social and economic characteristics; knowledge of RH-related topics (fertility, contraception, STIs/HIV/AIDS, HIV counseling and testing (HCT)) and patterns of RH services utilization.
Data was collected by researcher and trained research assistants. Research assistants were recruited and trained on the study objective, questionnaire content and how to ensure privacy and confidentiality. The collected data was checked for incompleteness and inconsistency and cleaned by researcher. One research assistant collects data in two sectors. In household with more than one adolescent aged 15-19 years, only one selected as potential respondents. All questionnaires and entered data will be kept secure by the researcher. Access is restricted. Name and addresses of participants were not required in the study.
Data Analysis
Data was checked for completeness, cleaned, coded and entered into excel sheet, and then exported to SPSS version 22.0 for further analysis. Frequencies and percentage were used to summarize descriptive statistics. Percentages were used to assess the level of RH knowledge and services utilization among rural adolescents. A total of 19 questions were used to assess knowledge of adolescents about reproductive health services. The right answer was scored 1 and wrong answer was scored 0, total scores were 19. The respondents were classified as good knowledge with scores >10 equivalent to 53% and lower knowledge with scores of 9 and less. Data were presented using tables and graphs accordingly. To determine the association between different factors associated with reproductive health knowledge and services utilization, a logistic regression model was employed. First, each variable was entered into a binary logistic regression model. Second, variables which showed significant at p-value of 0.05 fitted into multiple logistic regression model to assess the relationship between reproductive health knowledge and services utilization. Variables that remained significant at p-value of 0.05 in the final multivariate logistic regression model were identified as independent factors associated with reproductive health knowledge and services utilization among adolescents in rural areas of Rwamagana District.
Ethical Consideration
Ethical clearance was obtained from the Ethical committee of Mount Kenya University. Permission was obtained from Rwamagana District administration. The objective of the study was explained to the respondents. Respondents were free to decline or withdraw their participation in the study. Signed consent was obtained from the parents of caregiver for adolescents aged less than 18 years old. Data collection was conducted after verbal consent from the respondents.
Results
Socio-Demographic Characteristics of Respondents
A total of 392 adolescents aged 15-19 participated in the study. Participants were from 10 sectors of Rwamagana District including fumbwe, Munyaga, Gahengeri, Munyiginya, Musha, Muyumbu, Mwulire, Nyakaliro, Nzige and Rubona. Socio-demographic characteristics of adolescents from 10 Rwamagana Sectors are presented in table 2.
Table 2. Socio-Demographic Characteristics of Adolescents| Variables | Frequency | Percentage |
|---|---|---|
| Gender | ||
| Male | 187 | 47.7 |
| Female | 205 | 52.3 |
| Age Group | ||
| 15-17 | 198 | 50.5 |
| 18-19 | 194 | 49.5 |
| Marital Status | ||
| Single | 367 | 93.6 |
| Cohabiting | 25 | 6.4 |
| Religion | ||
| Catholic | 140 | 35.7 |
| Muslim | 118 | 30.1 |
| Protestant | 134 | 34.2 |
| Occupation | ||
| Student | 125 | 31.9 |
| Farmer | 50 | 12.8 |
| Merchant | 112 | 28.6 |
| Unemployed | 59 | 15.1 |
| Housewife | 46 | 11.7 |
| Education level | ||
| No formal education | 106 | 27.0 |
| Primary | 84 | 21.5 |
| Secondary | 202 | 51.6 |
| Current Schooling | ||
| In School | 232 | 59.2 |
| Out of school | 160 | 40.8 |
| Age of mother | ||
| 30-39 | 88 | 22.4 |
| 40-49 | 212 | 54.1 |
| 50-59 | 76 | 19.4 |
| 60+ | 16 | 4.1 |
| Mother Education | ||
| No formal education | 182 | 46.4 |
| Primary | 141 | 36.0 |
| Secondary | 39 | 9.9 |
| Tertiary | 30 | 7.7 |
| Socio-Class | ||
| Category 1 | 43 | 11.0 |
| Category 2 | 188 | 48.0 |
| Category 3 | 161 | 41.0 |
| Living status | ||
| With parents | 202 | 51.5 |
| With no parents | 190 | 48.5 |
| Living with | ||
| Mother only | 162 | 41.3 |
| Family member | 3 | 0.8 |
| Other ( partners) | 25 | 6.4 |
Socio-demographic characteristics of adolescents from Rwamagana District presented in table 4 shows that 205(52.3%) of them were female, half of them 198(50.5) were aged 15-17 years old. Of 392 adolescents 367(93.6%) were single, 140(35.7%) were affiliated to catholic religion, 125(31.9%) were students, 202(51.6%) completed secondary school while 232(59.2%) were currently at school.
Regarding the socio-demographic of their family, the majority 54.1% had mothers aged 40-49 years old, nearly a half 182(46.4%) reported that their mother had no formal education, 188(48.0%) were in ubudehe category 2, 202(51.5%) reported that they live with their parents, of those who do not live the parent 162(41.3%) were living with their mothers only.
Reproductive Health Knowledge among Adolescents in Rwamagana District
Individual knowledge about reproductive health aspects were assessed by 18 questions. Overall knowledge was also estimated.
Findings presented in table 3 shows that the majority of adolescents 180(54.1%) never heard that reproductive health services are offered at health center. Regarding individual knowledge on the reproductive health aspects a total of 166(42.3%) reported that a girl could become pregnancy at the first sexual intercourse, 225(57.4%) agreed that a girl could become pregnancy during puberty, 254(64.8%) agreed that a girl could become pregnancy after puberty.
Table 3. Reproductive health knowledge among the adolescents in rural area of Rwamagana District| Variables | Frequency | Percentage |
|---|---|---|
| Ever heard that reproductive health services are offered at health center | ||
| Yes | 212 | 45.9 |
| No | 180 | 54.1 |
| A girl could become pregnancy at first sexual intercourse | ||
| Yes | 166 | 42.3 |
| No | 226 | 57.7 |
| A girl could become pregnancy during puberty | ||
| Yes | 225 | 57.4 |
| No | 167 | 42.6 |
| A girl could become pregnancy after puberty | ||
| Yes | 254 | 64.8 |
| No | 138 | 35.2 |
| Males could be physically mature to get a girl pregnant | ||
| Yes | 254 | 64.8 |
| No | 138 | 35.2 |
| Males get a girl pregnant during puberty | ||
| Yes | 288 | 73.5 |
| No | 104 | 26.5 |
| Breast development for a girl is a sign of maturity | ||
| Yes | 339 | 86.5 |
| No | 53 | 13.5 |
| Appearance of public hair for both girls and boys is a sign of maturation | ||
| Yes | 301 | 76.8 |
| No | 91 | 23.2 |
| Appearance of facial hair development for boys is a sign of maturation | ||
| Yes | 233 | 59.4 |
| No | 159 | 40.6 |
| Appearance of menstruation for a girl is a sign of maturity | 325 | 82.9 |
| Male voice changes is a sign of maturity | 295 | 75.3 |
| Body shape changes for both girls and boys is a sign of maturity | 278 | 70.9 |
| Increasing of testicular size, acne and body odor are the signs of maturity | 312 | 79.6 |
| Ways of preventing unwanted pregnancy | ||
| Consistent and proper use of condom | 368 | 93.9 |
| use of oral contraceptive pills | 300 | 76.5 |
| use of Injectable contraceptives | 347 | 88.5 |
| use of long-lasting contraceptives | 179 | 45.7 |
| Aware about Sexually transmitted infections ( STIs) | 329 | 83.9 |
| STIs Symptoms | ||
| Pain during urination | 137 | 34.9 |
| Pain during sexual intercourse | 316 | 80.6 |
| Route of HIV transmission | ||
| Unprotected sexual intercourse | 371 | 94.6 |
| HIV can be got during the first unprotected sexual experience | 187 | 47.7 |
| Transfusion of infected blood | 191 | 48.7 |
| Sharing sharps | 325 | 82.9 |
| During child birth | 248 | 63.3 |
| During breastfeeding | 118 | 30.1 |
| Prevention of HIV | ||
| Sexual abstinence | 386 | 98.5 |
| Consistent and proper use of condom | 392 | 100 |
| Avoid transfusion with infected blood | 300 | 76.5 |
Concerning the maturity of male to pregnant a girl, 254(64.8%) reported that male could be physically mature to get a girl pregnant, 288(73.5%) reported that male get a girl pregnant during puberty. The majority of respondents 339(86.5) agreed that breast development for a girl as a sign of maturity, 301(76.8) said that appearance of public hair for both girls and boys is a sign of maturation, 233(59.4%) of respondents knew appearance of facial hair development for boys is a sign of maturity. It was observed that the majority of adolescents in Rwamagana District knew the sign of maturity where 82.9%, knew that appearance of menstruation for a girl as a sign of menstruation, 75.3% knew that male voice changes as a sign of maturity, 70.9% knew that body shape changes for both girls and boys is a sign of maturity and 79.6% knew that increase of testicular size, acne as sign of maturity.
In terms of knowledge about the ways of preventing unwanted pregnancy, the majority of respondents 93.9% knew that consistent and proper use of condom, 76.5% knew that use of oral contraceptive pills, 88.5% knew that use of injectable contraceptive should be used to prevent unwanted pregnancy.
Regarding the symptoms of STIs, only 34.9% knew that pain during urination can be STI symptoms, the majority 80.6% knew that pain during sexual intercourse is STI sign. For HIV transmission route, the majority 94.6% knew that HIV can be transmitted during unprotected sex, 82.9% knew that HIV can be transmitted through the sharing sharps. Adolescents were aware about HIV prevention measures where 386(98.5%) agreed that sexual abstinence during adolescents should prevent adolescent to get HIV, all of respondents knew that consistent and proper use of condom can prevent HIV.
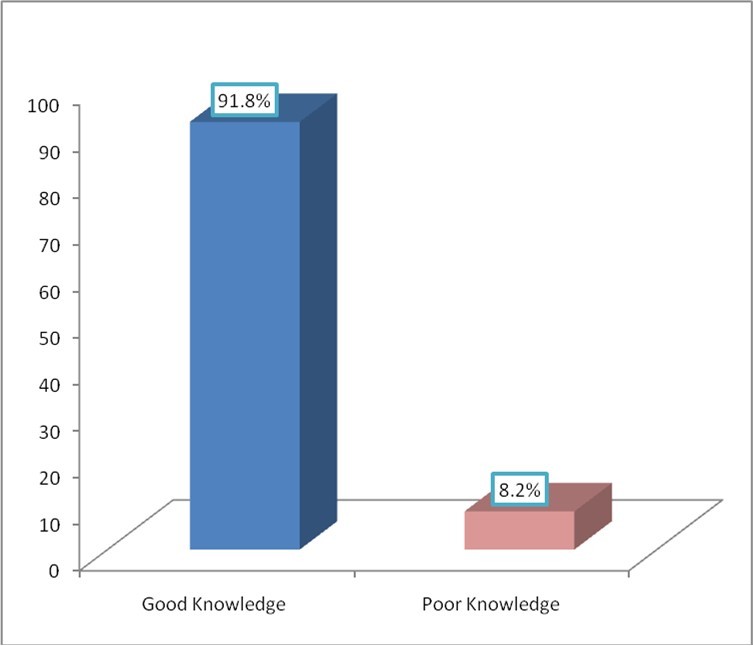
The findings presented in figure 1 shows that the majority of adolescents 91.8% had good knowledge about reproductive health.
Reproductive Health Services Utilized by Adolescent in Rural Area of Rwamagana District
The findings presented in table 4 indicated that the majority of adolescents 262(66.8%) had ever utilized reproductive health services at health facility. A total of 217(55.5%) had visited reproductive health center in the last 6 months, of those who visited the center 131(60.4%) were tested for HIV and given counseling, 151(55.5%) received STI diagnosis while very few adolescents 8(2.0%) visited RHS to seek for HIV treatment.
Table 4. Reproductive health services utilization| Variables | Frequency | Percentage |
|---|---|---|
| Ever utilize reproductive health services | ||
| Yes | 262 | 66.8 |
| No | 130 | 33.2 |
| Visit of RHS center in the last 6 months | ||
| Yes | 217 | 55.5 |
| No | 175 | 55.5 |
| Reasons for visit RHS center | ||
| HIV testing and counseling | 131 | 60.4 |
| HIV treatment | 11 | 5.1 |
| STI diagnosis | 151 | 55.5 |
| STI treatment | 8 | 2 |
| Obstacle to adolescent reproductive health services utilization | ||
| Never thought of the services | 44 | 11.2 |
| Services not necessary | 332 | 84.7 |
| Lack of knowledge on the services | 241 | 61.5 |
| Young people are healthy | 303 | 77.7 |
| Ever discuss with parents about reproductive health topics | ||
| Yes | 213 | 54.3 |
| No | 179 | 45.5 |
| Reasons for not discussing reproductive health topics with parents ( 179) | ||
| Not necessary | 111 | 62 |
| Fear of parents | 158 | 88.3 |
| Cultural restriction | 151 | 38.4 |
| Other reasons( parents not give us time, parents are busy, parents lack knowledge about the services | 141 | 78.8 |
| Distance to nearby RH service delivery | ||
| 0-1 km | 113 | 28.8 |
| 2-4 km | 195 | 49.7 |
| >5km | 84 | 21.4 |
| Walking time to reach RH service delivery | ||
| 30 min | 187 | 47.7 |
| One hour | 121 | 30.9 |
| Two hours | 62 | 15.8 |
| >2hours | 22 | 5.6 |
Adolescents also mentioned obstacle that limit them to seek for reproductive health service, a total of 332(84.7%) said that reproductive health service are not necessary to them. Lack of knowledge on the reproductive health services available for adolescent (61.5%) was mentioned as barrier to service utilization, 303 (77.7%) said that adolescent look healthy, therefore no need of seeking service. The majority 213(54.3%) of adolescents had discussed with parents about reproductive health topics. The reasons for not discussing reproductive health topics with the parents were mentioned where the majority 158(88.3%) reported that they fear to discuss reproductive health topics with the parents. Cultural restriction (38.4%) was also reported as barrier to discuss reproductive health topics with parents. The majority of adolescents 141(78.8%) reported that parents do not give them time to discuss reproductive health topics, parents are always busy and some parents lack knowledge about reproductive health.
Nearly a half 195(49.7%) of adolescent live at 2-4 km from the nearby reproductive health service delivery, 21.4% live at more than 5 km from health facility with adolescent reproductive health services. In terms of walking to health center, 47.7% used 30min to reach nearest health center, 5.6% used more than 2 hours Table 5.
Table 5. Bivariate analysis of the factors associated with reproductive health services utilization| Variables | Use of reproductive health services in the last 6 months | P-value | |
|---|---|---|---|
| Yes n(%) | No n(%) | ||
| Gender | 0.758 | ||
| Male | 102(47.0) | 85(48.6) | |
| Female | 115(53.0) | 90(51.4) | |
| Age Group | 0.744 | ||
| 15-17 | 108(49.8) | 90(51.4) | |
| 18-19 | 109(50.2) | 85(48.6) | |
| Marital Status | 0.727 | ||
| Single | 204(94.0) | 163(93.1) | |
| Cohabiting | 13(6.0) | 12(6.9) | |
| Religion | 0.009 | ||
| Catholic | 63(29.0) | 77(44.0) | |
| Muslim | 71(32.7) | 47(26.9) | |
| Protestant | 83(38.2) | 51(29.1) | |
| Occupation | 0.015 | ||
| Student | 61(28.1) | 64(28.1) | |
| Farmer | 31(14.3) | 19(10.9) | |
| Merchant | 75(34.6) | 37(21.1) | |
| Unemployed | 30(13.8) | 29(16.6) | |
| Housewife | 20(9.2) | 26(14.9) | |
| Education level | <0.001 | ||
| No formal education | 63(29.0) | 43(24.6) | |
| Primary | 60(27.6) | 24(13.7) | |
| Secondary | 94(43.3) | 108(61.7) | |
| Current Schooling | 0.051 | ||
| In School | 119(54.8) | 113(64.6) | |
| Out of school | 98(45.2) | 62(35.4) | |
| Age of mother | <0.001 | ||
| 30-39 | 60(27.6) | 28(16.0) | |
| 40-49 | 100(46.1) | 112(64.0) | |
| 50-59 | 51(23.5) | 25(14.3) | |
| 60+ | 6(2.8) | 10(5.7) | |
| Mother Education | 0.204 | ||
| No formal education | 93(42.9) | 89(50.9) | |
| Primary | 87(40.1) | 54(30.9) | |
| Secondary | 19(8.8) | 20(11.4) | |
| Tertiary | 18(8.3) | 12(6.9) | |
| Socio-Class | 0.084 | ||
| Category 1 | 19(8.8) | 24(13.7) | |
| Category 2 | 114(52.5) | 74(42.3) | |
| Category 3 | 84(38.5) | 77(44.0) | |
| Living status | 0.039 | ||
| With parents | 122(56.2) | 80(45.7) | |
| With no parents | 95(43.8) | 95(54.3) | |
| Distance from/too nearby RH service delivery | 0.04 | ||
| 0-1 km | 70(32.3) | 43(24.6) | |
| 2-4 km | 110(50.7) | 85(48.6) | |
| >5km | 37(17.1) | 47(26.9) | |
| Time | |||
| Discussion with parents about reproductive health services | 0.67 | ||
| Yes | 120(55.3) | 93(53.1) | |
| No | 97(44.7) | 82(46.9) | |
Factors Associated with Reproductive Health Services Utilization among Adolescents in Rwamagana District
In bivariate analysis religion (p=0.009), occupation (p=0.015), education level (p<0.001), age of mother (p<0.001), living status (p=0.039), and distance from/too nearby RH service delivery (p=0.040) were associated with use of reproductive health services in the last 6 months. Female (53.0%) were more likely to use reproductive health services than males, a half of respondents 50.2% who used reproductive health services in the last 6 months were aged 18-19 years old. Most of adolescent who used reproductive health services in the last 6 months were Protestants, currently in schools and live with their parents.
Variables with significant association in bivariate analysis (p-value less than 0.05) were taken to multivariate analysis.
The findings presented in table 6 shows the factors associated with reproductive health utilization among adolescent in Rwamagana District. The findings from multivariate analysis showed that adolescents who are affiliated to catholic church were less likely to use reproductive health services compared to protestant (aOR=0.447, 95%CI: 0.256-0.780, p=0.005). It was observed that adolescents who live with their parents were more likely to use reproductive health services compared to those who do not live with parents (aOR=2.161, 95%CI: 1.162-4.021, p=0.015).
Table 6. Multivariate analysis of the factors associated with reproductive health services utilization| aOR | 95%CI | P-value | |
| Religion | |||
| Catholic | 0.447 | 0.256-0.780 | 0.005 |
| Muslim | 0.822 | 0.474-1.424 | 0.485 |
| Protestant | Ref. | ||
| Occupation | |||
| Student | 1.072 | 0.422-2.721 | 0.884 |
| Farmer | 0.581 | 0.126-2.673 | 0.486 |
| Merchant | 1.102 | 0.418-2.907 | 0.845 |
| Unemployed | 0.968 | 0.394-2.375 | 0.943 |
| Housewife | Ref. | ||
| Education level | |||
| No formal education | 2.551 | 0.842-7.724 | 0.098 |
| Primary | 4.387 | 0.911-21.119 | 0.065 |
| Secondary | Ref. | ||
| Age of mother | |||
| 30-39 | 2.420 | 0.693-8.455 | 0.166 |
| 40-49 | 1.807 | 0.503-6.483 | 0.364 |
| 50-59 | 2.170 | 0.565-8.329 | 0.259 |
| 60+ | Ref. | ||
| Living status | |||
| With parents | 2.161 | 1.162-4.021 | 0.015 |
| With no parents | Ref. | ||
| Distance from/too nearby RH service delivery | |||
| 0-1 km | 1.542 | 0.846-2.810 | 0.158 |
| 2-4 km | 1.454 | 0.747-2.832 | 0.271 |
| >5km | Ref. |
Despite no significant association observed, adolescents with no formal education were two times more likely to utilize reproductive health services compared to those with secondary education. Similarly, adolescents with mothers aged 30-39 years were more likely to use reproductive health services. Adolescents who live nearest health facility were 1.5 more likely to use reproductive health services but no significant association observed.
Discussion
Adolescent’s reproductive health knowledge are affected by different controversies including says that adolescents are not ready for sensitive sexual information, comprehensive sexual education promote early sex, reproductive health education makes young people promiscuous, reproductive health education does not fit with our culture or religion, adolescent should not use contraceptive methods and adolescent should abstain from sex until marriage 11. Access and use of reproductive health services by adolescents, adolescents’ level of knowledge in RH is paramount. Increasing adolescent’s awareness about SRH and advocating for them is a crucial to the adolescent’s reproductive health effort. Hence, this study assesses the SHR knowledge and services utilization among adolescents in Rwamagana District.
The study found that more than a half of respondents 54.1% were not aware that reproductive health services are offered at health center. A total of 64.8% knew that a girl could become pregnancy after puberty, 73.5% knew that a male could get a girl pregnant during puberty. Adolescents in this study were knowledgeable about the signs of maturity for both girls and boys where 86.5% knew that breast development for a girl is a sign of maturity, 76.8% knew that appearance of public hair for both girls and boys is a sign of maturity, and appearance of menstruation for a girl is a sign of maturity. These findings are consistent with a study conducted in Ethiopia where 53.5% of the adolescents who participated in the study responded that a girl could get pregnant the first time she had sex and the age at which it could occur was mentioned as during puberty. The same study reported that the male counterpart could be mature of physically made a girt pregnant during puberty 3.
In contrast, a study conducted in China reported that the majority of adolescents had lower knowledge about fertility issues. The results from the Chinese study revealed that unmarried migrants demonstrated low levels of RH knowledge on pregnancy fertilization (29.4%) and contraception (9.1%). Females’ participants showed more knowledge about pregnancy, contraception and STDs, but with less knowledge on family planning policy than the male participants. Participants aged 15-19 years old had the least knowledge on pregnancy and family planning policy 12.
Regarding the reproductive health utilization, this study found that the majority of adolescents 66.8% have ever utilize reproductive health service, 55.5% responded that they visited reproductive health center in the last 6 months prior to the survey. This study showed that there is a significantly higher RH services utilization rate among rural adolescents when it is compared with the study undertaken in Jimma where 41.1% ever experienced the services 13 even though the latter finding is not more comparable as it was undertaken in urban setting.
In bivariate analysis religion, occupation education level, age of mother and living status were associated with use of reproductive health services (P<0.005). This finding are consistent with that conducted in Ethiopia where in bivariate analysis, the factor found to be significantly associated with reproductive health service utilization were education level and living status. In contrast, the same study found that adolescents age, marital status ; mothers’ educational status; poor family communication habit on SRH issues; family monthly income; history of sexual intercourse; poor discussion on SRH matters with sexual partner, pears, and health workers; perception of risk towards HIV/AIDS were associated with reproductive health services utilization 13. The inconsistence may be due to that Ethiopian study was conducted only among female aged 15-24 while this study was conducted among both male and female aged 15-19 years old.
It was observed that adolescents who live with their parents were more likely to use reproductive health services compared to those who do not live with parents (aOR=2.161, 95%CI: 1.162-4.021, p=0.015). In contrast, a study conducted in Ethiopia found that factors such as age of 16–20 years (AOR = 1.85, 95%CI: 1.17–2.92), mother’s educational status (being illiterate (AOR = .33, 95%CI:. 14–.77)), discussion about reproductive health services with their family (AOR = 8.02, 9%CI:5.52–11.66), being Merchant (AOR = 2.7995%CI:1.11–6.96), unemployed (AOR = 2.90, 95%CI:1.19–7.06) or student (AOR:2.38, 95%CI:1. 04–5.42) in occupation, high perceived severity (AOR = 4.05, 95%CI:2.68–6.11), high perceived barriers (AOR = .44, 95%CI:.30–64) were independent predictors of reproductive health services utilization among female adolescents the study area 14. The difference may due to the methodology mainly sample size where 844 female participated in the study while in this study 392 adolescent from one district were included in the study.
Conclusion
Majority of the adolescents demonstrated higher knowledge about reproductive health services in the study area. Moderate reproductive health services utilization by adolescents in Rwamagana District was observed. This study indicates that less than 60% of adolescents have visited reproductive health center in the last 6 months despite the availability of the services in the study area. The findings from multivariate analysis showed that adolescents who are affiliated to Catholic Church were less likely to use reproductive health services compared to protestant. It was observed that adolescents who live with their parents were more likely to use reproductive health services compared to those who do not live with parents. Parents need to increase the time they spend with their adolescents at home, and improve the discussion on the issues related to reproductive health. Adolescents are encouraged to visit health centers and youth centers in order to be know the services that are available for them at those centers.
References
- 1. (2005) WHO: World Health Organization and Deutsche Gesellschaft fuer Technische Zusammenarbeit (GTZ) GmbH. Sexually transmitted infections among adolescents: the need for adequate health services. Geneva: WHO Library Cataloguing-in-Publication Data.
- 3.Abajobir A A, Seme A. (2014) Reproductive health knowledge and services utilization among rural adolescents in east Gojjam zone, Ethiopia: a community-based cross-sectional study.BMC Health Serv Res.14:. 138.
- 4.Butler. (2003) The reproductive health situation of adolescents, 64 edition. Progress in Reproductive Research; 21-23.
- 5.Ayalew T, Yeshigeta. (2009) Adolescent Reproductive Health Services. in Jimma City: Accessibility and UtilizationEthiop J Health Sci.19(2) .
- 6. (2007) WHO: Adolescent pregnancy-Unmet needs and undone deeds: A review of the literature and programmes: Issue in Adolescent Health and Development.
- 7.Abiodun O, Olu-Abiodun O, Ani F, Sotunsa O.. Sexual and Reproductive Health Knowledge and Service Utilization among In-school Rural Adolescents in Nigeria.J AIDS Clin Res2016 7-6.
- 11. (2017) UNFPA: Integrating Comprehensive Sexuality Education (CSE) in Teacher’s Guides and Students Textbooks.
- 12.Liu Z, Zhu M, Dib H H, Li Z, Shi S et al. (2011) RH knowledge and service utilization among unmarried rural-to-urban migrants in three major cities, China.BMC Public Health11: 74.
Cited by (6)
This article has been cited by 6 scholarly works according to:
Citing Articles:
BMC Public Health (2025) OpenAlex
BMC Public Health (2025) Crossref
Julienne Nyirarukundo, Venuste Musugire, Boniface Nsengiyumva, Joella Mukashyaka, Zephanie Nzeyimana - BMC Public Health (2025) Semantic Scholar
Frontiers in Reproductive Health (2024) OpenAlex
Frontiers in Reproductive Health (2024) Crossref
Sri Wahyuningsih, Sri Widati, S. Praveena, Mohammad W. Azkiya - Frontiers in Reproductive Health (2024) Semantic Scholar
Communications Biology (2023) OpenAlex
Communications Biology (2023) Crossref
Chandrasekhar Yadavalli, Sathisha Upparahalli Venkateshaiah, Sandeep Kumar, H. Kandikattu, Lokanatha Oruganti et al. - Communications Biology (2023) Semantic Scholar

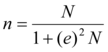 Where n is desired sample, N target population, e is the marginal error (5%)
Where n is desired sample, N target population, e is the marginal error (5%)